Couples with an unfulfilled desire to have children have the option of having their fertility tested. Learn about various types of fertility tests that can help provide clarity.
Whether you have been trying to conceive or are just curious about your fertile potential, having a better understanding of your fertility can be helpful.
From at-home testing to imaging procedures performed by a doctor, a wide variety of fertility tests is available. Fertility can be tested by hormone tests, tissue samples that are examined in the laboratory, ultrasound imaging, and other methods. Various factors, such as general health and medical history, the menstrual cycle, medical conditions, whether and how long a couple has been trying to get pregnant, and whether there have been previous pregnancies, all play a role in test selection. It is best for an individual or couple to seek advice from a fertility specialist regarding which test is most suitable for their case.
Who are fertility tests suitable for?
Fertility tests are suitable for anyone who wants to find out more about their fertility. For both sexes, testing usually begins with a urine sample and blood testing. Women may also have a gynecological exam that evaluates the internal reproductive organs and an ultrasound to visualise internal functioning and health. Men will then have a semen analysis to assess sperm and semen parameters. These tests provide valuable information about the state of hormones and other health conditions.
Fertility tests can give an assessment of the current fertility situation. For example, if a woman is found to still have a large ovarian reserve (remaining number of eggs), she often has a longer timeframe in which she could become pregnant. If fewer eggs are estimated to remain, pregnancy should ideally be attempted sooner. However, according to reproductive medicine, this prognosis is only reliable to a limited extent, as it is only a snapshot.
Fertility tests and analyses can also be used to determine the possible causes of an inability to conceive, and to suggest treatment options or next courses of action.
Common fertility tests for women
The most common identifiable causes of female infertility include ovulation disorders, tubal blockages or other diseases of the reproductive organs, such as irregular cervical mucus production or endometriosis. A series of fertility tests can reveal where the problem lies so that the best possible treatment can then be applied. In most cases, hormone tests are done first. More specific testing methods can then be used. The most important test methods are outlined below.
Initial hormone tests
Measuring hormone levels can provide important information about a woman's fertility. Ideally, the blood sample for such tests should be taken between the second and fifth day of the female cycle (which is the second to fifth day after menstruation begins). All hormones associated with the menstrual cycle are examined: luteinising hormone (LH) and follicle-stimulating hormone (FSH), those of the thyroid gland (TSH), the breastfeeding hormone prolactin, progesterone, as well as the hormones estradiol (a form of estrogen made by the ovaries) and testosterone.
These hormone levels provide information about a woman’s reproductive health. Values that are too high or too low can indicate an imbalance. Certain patterns in these hormones can also suggest disorders, such as polycystic ovary syndrome (PCOS).
At-home tests of certain hormones are also available. For example, a home ovulation test measures luteinising hormone and is able to detect when a woman could potentially get pregnant. It works in a similar way to a pregnancy test: the test strip has to be exposed to urine, and and the result is shown with the coloured lines. If the test is positive, this indicates that it is a good time for a woman to try to conceive.
Anti-Müllerian hormone (AMH)
A key part of ovarian reserve testing, AMH is measured by a blood test. Measuring anti-Müllerian hormone can provide information about how many potentially fertilisable eggs are still present in a woman's ovaries. The granulosa cells in the ovaries produce AMH during the reproductive years, i.e. between puberty and menopause. These cells surround the growing follicles, whose role is to help to nurture and release a fertilisable egg after it has matured, in the process of ovulation.
AMH regulates follicle growth, and the AMH level correlates with the number of follicles in the ovary. This means that the more remaining eggs there are in the ovaries, the higher the level of this hormone.
This test is particularly useful in clarifying possible female infertility. If assisted reproductive techniques, such as intrauterine insemination (IUI) or in vitro fertilisation (IVF), are being considered for conception, the AMH value can be used to assess how well the ovaries are likely to respond to hormonal stimulation. How near a woman’s menopause may be can also be estimated on the basis of this hormone.
Other tests
The post-coital test (PCT)
The post-coital test is used by gynecologists to assess cervical mucus. Specifically, it is used to check whether the mucus is receptive to sperm around the time of ovulation. Usually, at this phase of the menstrual cycle, the cervical mucus becomes similar to egg white in consistency; this helps sperm to move through the cervix and into the uterus and fallopian tubes to fertilise the egg.
The PCT test is conducted 6–12 hours after sexual intercourse. It examines how many sperm are present in a sample of cervical mucus. In this way, possible obstacles to fertilisation can be investigated.
For example, the test result may show that the cervical mucus is too thick, preventing sperm from passing through. This, in turn, may indicate a hormonal imbalance. It may also be that there are hardly any sperm cells to be found in the mucus—an indication that male fertility may be limited.
Ultrasound imaging
An ultrasound can be performed either over the lower abdomen, or in transvaginal form by inserting an ultrasound wand into the vagina. It can provide information about the uterus (e.g. whether there are abnormalities in its shape, or growths known as fibroids) and the ovaries (e.g. whether they contain multiple small cysts, in the case of suspected PCOS).
Hysterosalpingography (HSG)
Hysterosalpingography, also known as a hysterosalpingogram, is an X-ray examination of the uterus and fallopian tubes. Specifically, it helps to assess the internal shape of the uterus for abnormalities. In addition, it checks whether the fallopian tubes are open. This is important because mature eggs need to travel through the fallopian tubes to the uterus following ovulation, and sperm need to be able to access the fallopian tubes from the uterus in order to fertilise eggs. Some conditions, such as pelvic inflammatory disease (PID), can lead to partial or complete blockage of the tubes.
In HSG, a contrast medium is injected into the female uterus via a thin catheter tube passed through the cervix. Next, a series of X-rays are performed. At first the uterus will appear white, because of the contrast medium. If the fallopian tubes are open, the contrast medium and white color should spread through the length of the fallopian tubes, and into the pelvic cavity.
Hystero-salpingo contrast sonography (HyCoSy)
As with a hysterosalpingogram, this test is performed to assess whether the fallopian tubes are open. However, it differs from HSG in that it doesn’t use X-ray and does not include any exposure to radiation. Instead, after a contrast medium is injected into the uterus as in HSG, the gynecologist inserts an ultrasound wand into the vagina to check the uterus as well as whether the fluid passes through the fallopian tubes.
Hysteroscopy (endoscopy)
During hysteroscopy, a hysteroscope—a long, slim telescope with a light at the end—is passed through the vagina and cervix, into the uterus. Gas or fluid are then sometimes introduced, via the hysteroscope, into the uterine cavity so that the doctor can view it more extensively. The procedure is particularly well-suited for detecting the cause of abnormal uterine bleeding.
It also can detecting fibroids, tumours or abnormalities in the uterine lining. When an abnormality is detected, it can sometimes be removed during the procedure. This is known as operative hysteroscopy.
Laparoscopy (laparoscopy)
A laparoscopy is a surgical procedure, done under general anesthetic. It is the most invasive of the imaging tests, and is usually done when there is a desire to collect tissue (biopsy) for testing or to confirm conditions such as endometriosis or pelvic inflammatory disease.
In this procedure, a thin lighted telescope known as a laparoscope is passed through an incision in the abdomen, where it can be used to examine the female reproductive organs, and diagnose conditions such as endometriosis, pelvic inflammatory disease, uterine fibroids or ovarian cysts. Some problems, such as fallopian tube scarring or ovarian cysts, can also be treated during the procedure.
Common fertility tests for men
In about 20–30% of infertility cases, male factors are found to be solely responsible, and they are found to contribute to about 50% of cases overall. Therefore, in couples who are unable to conceive, it is important that the male partner also has his fertility checked. The most common causes of male infertility are hormonal disorders, sperm transport disorders, low sperm quantity and poor sperm quality. The most important methods of male fertility testing are outlined below.
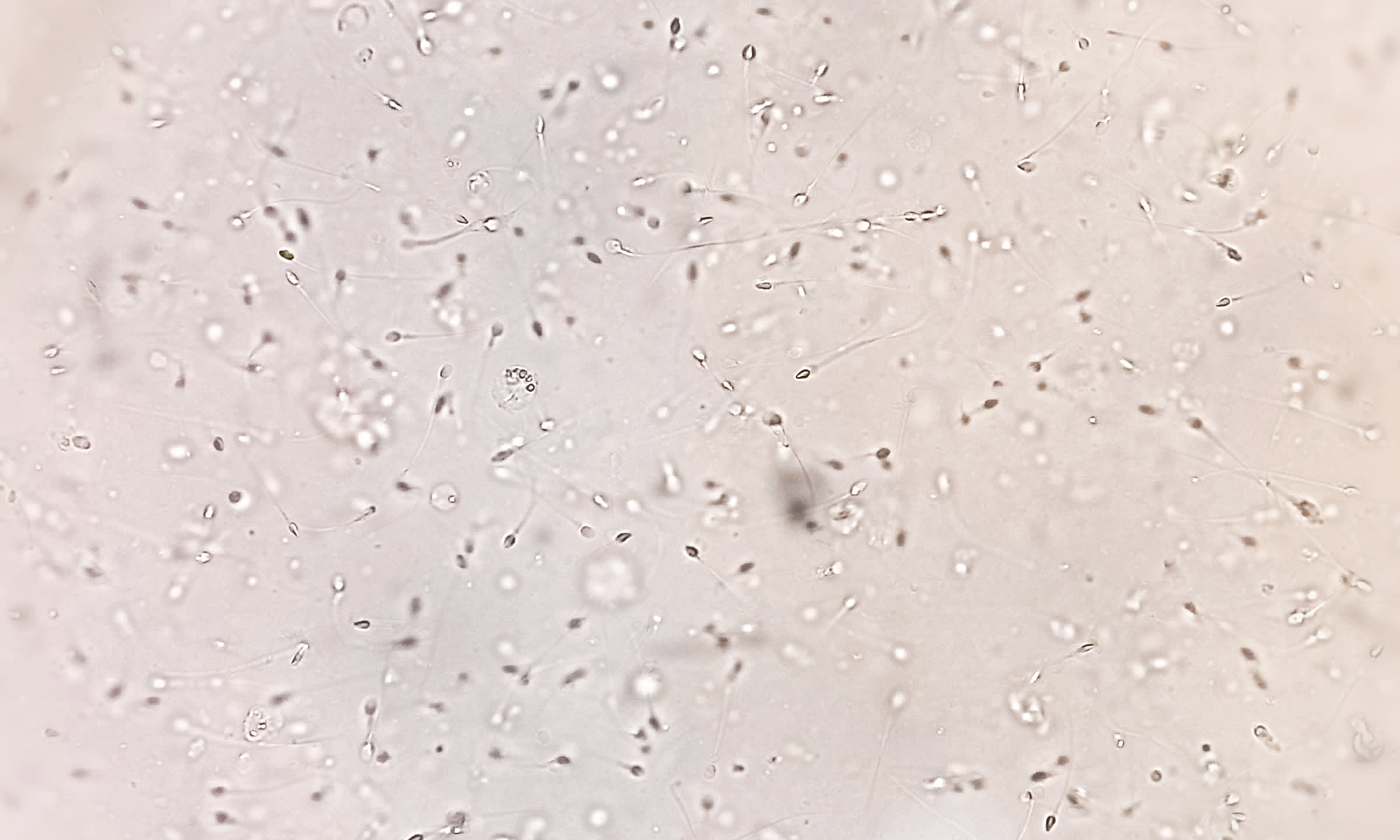
Semen analysis
A semen analysis can provide important information about a man's fertility. The semen sample for this test is obtained by the man through masturbation. It is subsequently examined in a laboratory to determine its quality. Aspects examined include:
- Semen volume
- pH level of the semen
- Sperm concentration (also known as sperm count - number of sperm per mililitre of semen)
- Sperm motility (ability to move efficiently)
- Sperm morphology (shape)
- Liquefaction: How quickly semen changes into a liquid
See our article for a more in-depth look at semen analysis.
Hormone tests
If the semen analysis shows a lack of sperm, it should be clarified whether there is a hormone imbalance. The testicles, where the sperm are produced, are controlled by hormones. These hormones can be examined by means of blood tests. The main hormone levels tested are:
- Follicle-stimulating hormone (FSH)
- Luteinising hormone (LH), which is involved in the maturation of the sperm
- Prolactin (may indicate an imbalance in the pituitary gland, which in turn may interfere with the production of FSH, testosterone and LH)
- Testosterone, produced in the testicles
Testicular biopsy
A testicular biopsy is a procedure in which a tissue sample is taken from the testicles and examined in the laboratory. If semen analysis has shown that there is little or no sperm, taking the sample directly from the testicles can reveal whether sperm are being produced but then prevented from being ejaculated (known as obstructive azoospermia) or whether they are not being produced at all (non-obstructive azoospermia). If this is the case, they can be obtained and examined in this way.
This procedure can also be used to extract sperm that can be frozen and/or used in fertility treatments such as in vitro fertilisation.
Ultrasound examination of the testicles
In addition to a semen analysis, the testicles can also be examined by means of ultrasound during an examination of male fertility. Assessment of the size, structure and tissue of the testicles can provide information about possible anatomical causes of an male infertility. For example, if the testicles are too small due to hypogonadism or if the scrotum contains varicose veins (varicocele), this can be reasons for an inability to conceive. The examination is also suitable for making inflammations, cysts or tumours visible. The blood supply can also be examined.
Another form of ultrasound examination suitable for men is transrectal ultrasound. With this method, the prostate and seminal vesicles are examined via a probe that is inserted into the anus. Because of the short distance, tumours and inflammations in this area can be located and examined more closely.
Takeaway
If a couple is unable to conceive on their own over a period of time (usually six to twelve months, depending on age), the cause should be investigated. Fertility testing offers ways to clarify the fertility of both partners. Various methods, including blood tests of hormone levels and imaging, can be performed in the two sexes. In men, semen analysis also forms a core part of fertility testing.
A fertility specialist can advise an individual or couple in terms of which tests may be appropriate, and in which order they should be done. When the test results indicate a need for treatment or intervention, a tailored plan can be designed.
Would you learn more about your fertility? Our team of fertility specialists will be happy to inform you about the available test options and, if necessary, provide you with concrete suggestions for treatment or further procedures. Reserve your spot for a free consultation today.