Considering TESE? In this article you will learn more about this sperm retrieval procedure, including its uses, benefits, and costs.
Key Facts:
- TESE is a surgical procedure used to obtain sperm directly from the testicles
- Small tissue samples are taken from the testicles and examined for sperm
- The sperm obtained by TESE are only suitable for intracytoplasmic sperm injection (ICSI)
- If sperm are present, the success rate for subsequent ICSI treatment is around 30%
- Micro-TESE and MESA are alternatives to TESE
Introduction
Testicular Sperm Extraction (TESE) is a medical procedure used when no sperm is detectable in the semen analysis. It is commonly applied in cases where men have few or no sperm cells in their seminal fluid (azoospermia), which can be due to various reasons.
This article provides important details on TESE, from its procedure to success rates and costs.
The TESE Procedure
During TESE, small tissue samples about the size of a pinhead are extracted through a surgical procedure under general anesthesia. This around 30-minute procedure is conducted by a urologist. The testicular tissue is then microscopically examined to identify and extract sperm.
If the testicular tissue reveals sperm capable of fertilisation, these can be cryopreserved for multiple attempts.
The sperm extracted through this method can only be used for Intracytoplasmic Sperm Injection (ICSI).

When is Testicular Sperm Extraction (TESE) used?
TESE is employed when a man has little to no sperm in his ejaculate due to congenital abnormalities, injuries, infections, or other factors that may interfere with sperm production or release. TESE is used for:
- Obstructive azoospermia: This condition occurs when the seminal ducts (such as the vas deferens, epididymis or seminiferous tubules) are blocked or narrowed, preventing sperm from being released.
- Cryptozoospermia: In cases of cryptozoospermia, only a few sperm can be detected in the ejaculate. The sperm count is so low that it is insufficient for natural fertilisation.
- Klinefelter syndrome: Over 95% of men affected by Klinefelter syndrome suffer from azoospermia. This condition cannot be cured, and the sperm count typically remains significantly reduced.
- Undescended testicles: If left untreated, undescended testicles, which are usually diagnosed and treated during childhood, can lead to infertility.
- Male sterilisation: TESE can benefit men who wish to have children again after a vasectomy. Even if there are no more sperm in the ejaculate, they are still preserved in the testicles.
- Chemotherapy: If sperm hasn't been cryopreserved before chemotherapy, it can be extracted from the testicles using TESE.
What is the success rate of TESE?
TESE’s success rate depends on several factors, including the underlying cause of sperm absence, the man's age, and other individual factors. If well-formed, motile sperm are found after TESE, the success rate for ICSI treatment is approximately 30%.
If no sperm are found after TESE, it is unfortunately not possible to conceive a biological child.
What are the possible risks and side effects of TESE?
Similar to any surgical procedure, TESE also presents certain risks. These may include:
- Infections
- Bleeding (in rare cases, secondary bleeding may occur)
- Bruising on the scrotum
- Pain or slight tension in the procedure area
What's the difference between TESE, micro-TESE, and MESA?
TESE, micro-TESE, and MESA are three separate sperm retrieval techniques for men suffering from infertility due to the absence of sperm in their ejaculate. Although these procedures share the same goal, their execution and application vary significantly.
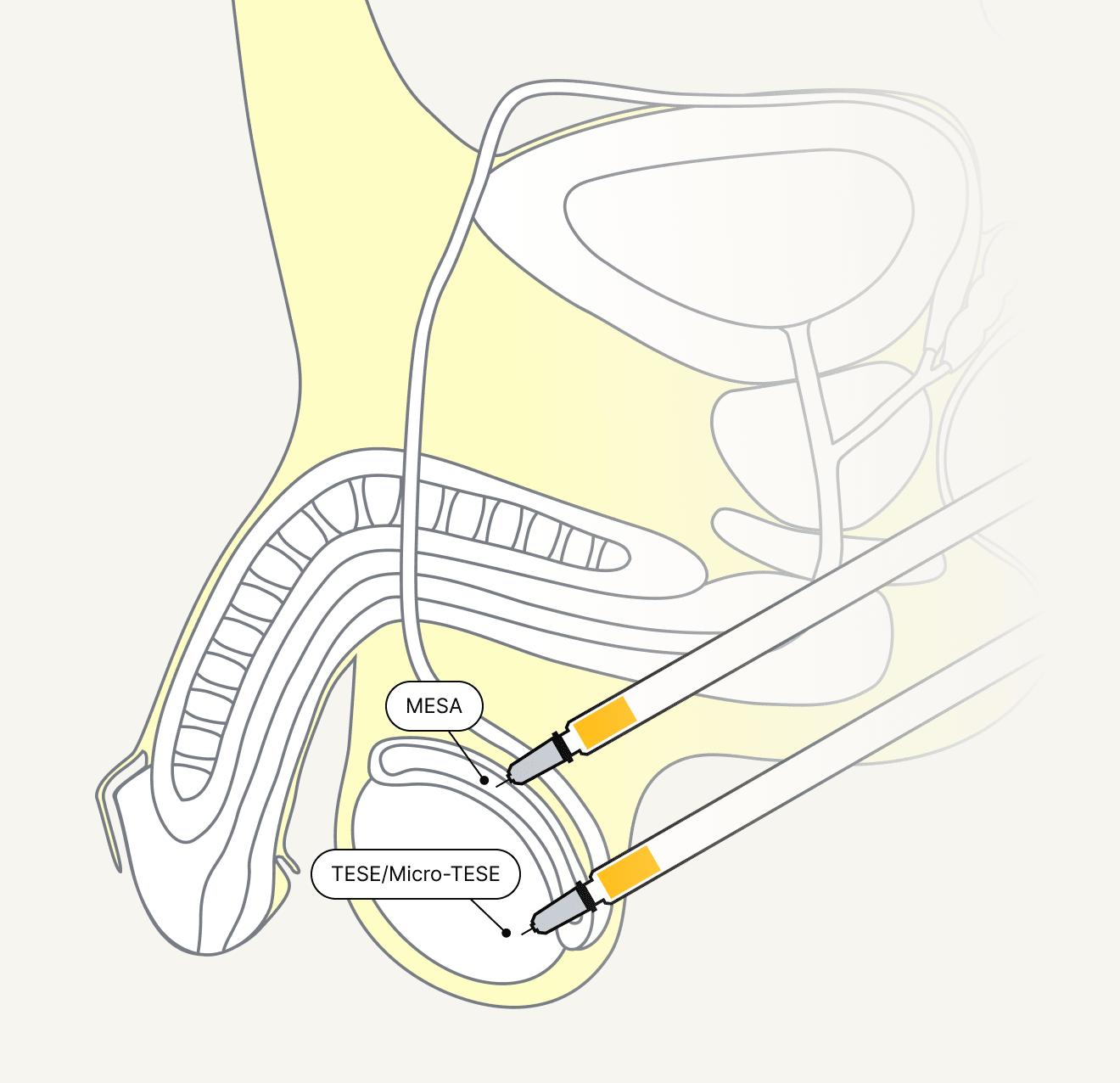
TESE (Testicular Sperm Extraction)
TESE is a surgical technique where tissue samples are directly extracted from the testicles to retrieve sperm. This method is typically employed when sperm cannot be found in the ejaculate due to blockages in the reproductive tract, congenital abnormalities, or other causes. The collected tissue samples are microscopically examined to identify and extract sperm, which can then be used for assisted reproduction.
Micro-TESE (Microsurgical Testicular Sperm Extraction)
Micro-TESE is a refined version of TESE that utilises a high-resolution microscope to examine the testicles in greater detail. Unlike conventional TESE, which extracts tissue from a large area, micro-TESE allows for more precise identification of areas of spermatogenesis in the testicles, potentially increasing the success rate of sperm retrieval. This technique is often employed in men for whom TESE has been unsuccessful previously or in whom the likelihood of finding sperm in the testis is low.
A study discovered that micro-TESE is often more successful than TESE. For instance, with micro-TESE, the chance of sperm retrieval in men with non-obstructive azoospermia can reach up to 60%, whereas with TESE, it hovers between 20 and 45%.
MESA (Microsurgical Epididymal Sperm Aspiration)
Unlike TESE and micro-TESE, which retrieve sperm from the testicles, MESA aims to obtain sperm directly from the epididymis. In this method, a small amount of fluid is drawn from the epididymis, which is then microscopically examined to locate and extract sperm. MESA is often used in patients who have no sperm in the ejaculate due to blockages in the epididymis.
According to a study, the live birth rate is significantly higher with ICSI preceded by MESA than with TESE (39% vs. 24%).
Can sperm from a TESE be used for other fertility treatments?
No, the number of sperm obtained from TESE is not sufficient for insemination (IUI) or IVF treatment to fertilise an egg. However, with ICSI, a single sperm capable of fertilisation is selected and injected directly into the egg.
What is the cost of a TESE?
The cost of TESE ranges from CHF 1,500 - 2,500, plus the cost of cryopreserving testicular tissue. Basic insurance typically does not cover these costs. If TESE is performed due to cancer, health insurance often covers cryopreservation.
Takeaway
TESE can be performed to obtain sperm from testicular tissue if no sperm is detected in the ejaculate. Other options include micro-TESE or MESA. The choice of procedure depends on the patient's individual circumstances, the cause of infertility, and the doctor's recommendation. A thorough consultation with a reproductive medicine specialist is crucial for the best possible treatment.
TESE is only suitable for ICSI. If healthy and motile sperm are found during TESE, the chances of successful pregnancy are as good as with conventional ICSI.
If you're interested in learning more about your sperm quality, consider a comprehensive fertility check. Most health insurance companies reimburse the cost of this test. To learn more, schedule a consultation appointment.







