IVF success rates can reach 40–50% under 35 but drop to 7–13% after 40. Discover the factors that shape your chances and what you can do to boost them.
Everything you need to know about IVF success rates:
- Under the age of 35, success rates are 40–50% per transfer; over 40, they drop to just 7–13%.
- Single embryo transfer drastically reduces risks for both mother and child.
- With normal sperm quality, IVF shows better results than ICSI.
- IVF treatment itself does not increase the risk of miscarriage – it corresponds to the age-specific natural rates.
- Preimplantation genetic testing allows for the targeted selection of chromosomally healthy embryos.
If you and your partner are considering in vitro fertilisation (IVF), one of the first questions you might ask is: What are my chances of success? IVF is one of the most widely used forms of medically assisted reproduction, and for many couples it offers real hope. Thanks to advances in reproductive medicine, outcomes have improved dramatically in recent years. But results vary, and factors such as a woman’s average age, egg quality, sperm health, and overall wellbeing all play an important role.
This article explains the current IVF success rates, how age and other factors affect your outcome, and what you can do to improve your own chances of success.
IVF Success: A Story of Progress
When IVF was first introduced in the early 1980s, the pregnancy rates per cycle were only around 6%. For couples facing infertility, that meant many attempts with little certainty of success. Today, however, IVF is one of the most effective forms of assisted reproductive technology.
In 2019, 5,993 couples underwent IVF or ICSI treatment, resulting in 2,204 live births — which corresponds to about 3% of all births in Switzerland. The vast majority of cycles were ICSI (84%), while conventional IVF accounted for 15%. Success rates are typically reported per embryo transfer or per cycle: for example, the live birth rate per embryo transferred was 21.2% after a fresh cycle and 24.1% after a frozen-thawed cycle.
This progress is due to:
- More precise ovarian stimulation that produces a higher number of oocytes and is tailored to each woman’s hormone levels and ovarian reserve.
- Advanced laboratory techniques such as ICSI (intracytoplasmic sperm injection), which allows fertilisation even with severe male infertility.
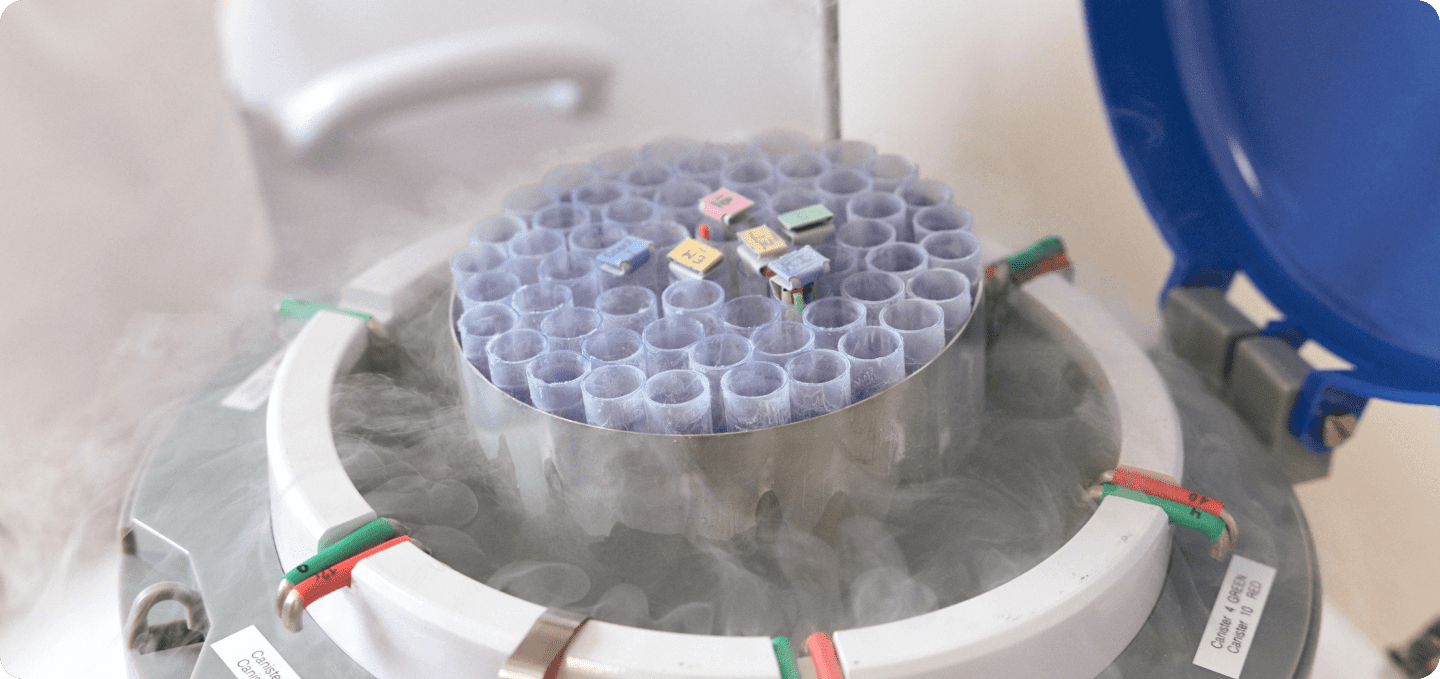
- Cryopreservation: with modern vitrification, more than 95% of frozen embryos survive and can be used in later transfer cycles.
Together, these developments have turned IVF into a cornerstone of modern human reproduction.
IVF Success Rates by Age
Despite these advances, a woman’s age remains the single most important factor for IVF success. Egg quality declines naturally over time, which reduces the likelihood of implantation and increases the risk of miscarriage.
- Under 35 years: Women in this group have the best outlook. The pregnancy rate per embryo transfer is about 40–55%, and cumulative birth rates reach up to 86% after several cycles.
- Ages 35–37: Success rates drop to around 25–40%. Swiss and US data show that live births occur in about 32% of cases in this age group, compared with 42% in women under 35.
- Ages 38–40: The rate falls further to 20–27%. At this stage, oocytes are more likely to carry chromosome abnormalities, which increase miscarriage risk. Data from the US confirm this trend: Among women aged 38 to 40, IVF treatments resulted in a live birth in only about 22% of cases – compared with nearly one third in women aged 35–37.
- Over 40 years: The chances of success fall sharply to 7–13% per cycle, while miscarriage rates climb to over 40%. For women aged 41–42, live birth rates are about 12%; by age 43–44 they drop to 5%, and over 44 they are just 1%.

IVF or ICSI – Which Is More Effective?
The development of ICSI revolutionised the treatment of male infertility by enabling fertilisation even with very poor sperm quality. However, when sperm quality is normal, conventional IVF can actually yield better outcomes:
- Fertilisation rates: 58% with IVF vs. 53% with ICSI
- Live births: 47% with IVF vs. 43% with ICSI
- First pregnancy: 33% with IVF vs. 27% with ICSI
This means ICSI is invaluable when male infertility is severe, but it is not automatically the better choice in every case.
What If It Doesn’t Work the First Time?
It’s common for couples to hope IVF will succeed on the first attempt. While that does happen, many need more than one transfer cycle. The first attempt typically results in pregnancy in 30–48% of cases, depending on age. But the chances of success increase significantly over time:
- After two cycles, 54–61% of couples achieve pregnancy.
- After three cycles, cumulative birth rates rise to 61–67%.
This is why most fertility specialists recommend planning several treatment cycles from the outset.
Key Advances in IVF
Cryopreservation of Embryos
Freezing embryos has transformed IVF treatment. Extra embryos from one cycle can be safely stored at -196°C and transferred later at the optimal time. This reduces the physical and emotional burden of repeated stimulation and allows couples more flexibility.
Single Embryo Transfer (SET)
In the past, transferring multiple embryos was common, which led to high rates of multiple births. Today, most clinics in Switzerland recommend single embryo transfer. According to the Federal Statistical Office (FSO), the rate of multiple pregnancies after IVF has dropped from 17.4% in 2002 to just 2.8% in 2023.
This reduction has enormous benefits, lowering the risks of premature birth, low birth weight, and pregnancy complications.
At the Cada fertility clinic in Zurich, we also follow this approach to ensure the safest possible outcome for both mother and child.
Lifestyle and Male Fertility: How You Can Make a Difference
While age and genetics can’t be changed, lifestyle has a clear impact on IVF outcomes. Research shows that nutrition, physical activity, sleep quality, and exposure to environmental toxins all influence fertility. A balanced diet rich in vegetables, whole grains, and healthy fats supports hormone balance and egg quality, while maintaining a healthy weight helps reduce risks. Avoiding smoking and reducing alcohol intake can also improve both oocyte and sperm health.
Supplements such as folic acid are strongly recommended before starting IVF, and some studies suggest antioxidants may support sperm quality. Regular but moderate exercise helps circulation and reduces stress, while good sleep habits support hormonal regulation.
It’s also important to look at male fertility. Poor sperm quality contributes to infertility in almost half of cases. In milder cases, insemination (IUI) may be recommended before moving to IVF or ICSI. In severe cases, ICSI is the best option because it bypasses natural barriers to fertilisation. Where sperm quality is extremely limited or absent, sperm donation may be discussed as an alternative, though it is carefully regulated in Switzerland. Addressing male fertility alongside female factors ensures couples achieve the best possible chances of success with IVF or ICSI.
Factors That Influence IVF Outcomes
Beyond age and lifestyle, other factors can influence IVF results:
- Egg reserve and hormones: Blood tests (AMH, FSH) and ultrasound scans determine the number of available oocytes.
- Embryo quality: Growing embryos to the blastocyst stage (Day 5) helps select the healthiest ones for transfer.
- Genetic testing: PGT-A and PGD allow for the detection of chromosome abnormalities, reducing miscarriage risk and improving success rates in selected cases.
Future Trends in Reproductive Medicine
The field of IVF is evolving rapidly, with several exciting innovations on the horizon.
- Artificial intelligence (AI): Algorithms can now analyse embryo development images more precisely than the human eye, predicting which embryos have the highest chance of implantation. AI is also being used to tailor hormone stimulation more accurately and to improve diagnostic imaging.
- Advances in PGT-A and PGD: Genetic testing of embryos is becoming more precise, allowing for earlier detection of abnormalities and increasing the chances of selecting healthy embryos. This reduces the number of failed cycles and miscarriages.
- Egg donation in Switzerland: The expected legalisation of egg donation under revisions to the Reproductive Medicine Act would mark a major milestone. This change would align Switzerland more closely with other European countries and could significantly increase overall birth rates, especially for women over 40.
- Policy and healthcare changes: Updates to the law may also affect coverage by health insurance and access to infertility treatments, making them more widely available through the Swiss healthcare system.
These developments will continue to shape assisted reproductive technology and improve outcomes for couples facing infertility.
How to Improve Your IVF Chances
Even though some factors are beyond your control, there are still many ways to increase your chances of success with IVF:
- Quit smoking and reduce alcohol consumption.
- Eat a nutrient-rich diet and maintain a healthy weight.
- Take folic acid and other recommended supplements before and during treatment.
- Stay physically active and prioritise good sleep.
- Manage health conditions such as diabetes, thyroid disorders, or endometriosis before treatment.
- Choose a clinic with proven expertise in reproductive medicine and a strong track record of birth rates.
Takeaway: Your Personal Outlook Matters Most
Thanks to progress in assisted reproductive technology, IVF is more successful than ever before. Even when circumstances are not ideal, modern methods make it possible for many couples to achieve their dream of parenthood.
But every situation is unique. Factors such as average age, ovarian reserve, sperm quality, and general health all influence your outcome. That’s why a personal consultation is essential.
Ready to understand your personal chances with IVF?
At Cada in Zurich, we’ll assess your individual situation, explain your options, and guide you through the treatment that best supports your path to pregnancy. Book your consultation today.
FAQ on IVF Success Rates
How many IVF attempts will I need to get pregnant?
The number of IVF attempts needed is individual and depends on age and the cause of infertility. Some women become pregnant on the very first attempt. Thanks to cryopreservation, multiple embryos can often be obtained from a single stimulation cycle and transferred later — this significantly increases the overall success rate without requiring another round of stimulation.
What are my chances of getting pregnant with IVF?
IVF success rates depend strongly on age and are usually reported per embryo transfer:
- Under 35 years: 40–50%
- 35–39 years: 30–40%
- Over 40 years: 15–25%
Over several cycles, the cumulative chances increase considerably.
Does IVF often work the first time?
Yes, especially for younger women. Under the age of 35, the chance of pregnancy in the very first IVF attempt is already 40–50%. With increasing age, success rates decline, but many couples still achieve their goal in subsequent cycles.
What are the risks of IVF treatment?
IVF is generally very safe. Possible risks include:
- Ectopic pregnancy: 1–3% (vs. 1% in natural pregnancies)
- Miscarriage: depends on age, but not increased by IVF itself
- Multiple pregnancies: Greatly reduced thanks to single embryo transfer, but still associated with higher risks of premature birth, low birth weight, and complications.







