Find out how hormonal contraception – like the pill or hormonal coil – might influence your ability to conceive.
What You Need To Know About Birth Control and Fertility
- Hormonal birth control does not cause infertility or increase the risk of birth defects.
- Most women resume menstruation within a couple of weeks.
- Hormonal contraceptives work by preventing ovulation and thickening cervical mucus.
- Hormonal implants rank among the most effective types of birth control.
- After stopping hormonal methods, irregular periods may return, especially in women with previously undiagnosed conditions like PCOS or endometriosis.
What You Should Know About Birth Control And Fertility
Hormonal birth control methods, such as contraceptive pills, the vaginal ring, or a hormonal intrauterine device (IUD), are widely used forms of contraception. But many wonder: can they impact your ability to get pregnant in the future? Here's what you should know about the link between hormonal birth control and fertility.
Still waiting for a positive test?
If you’ve been trying to conceive for a while now without success, it’s time to take the next step. Book your personalized fertility analysis at our leading fertility clinic in Zurich.
What Are the Main Types of Birth Control?
Contraceptive methods are generally divided into hormonal and non-hormonal options.
Non-Hormonal Methods
Non-hormonal contraception includes:
- Barrier methods such as condoms, female condoms (Femidom), diaphragms, cervical caps and contraceptive gels.
- Other options like the copper IUS (IUD) and fertility awareness methods.
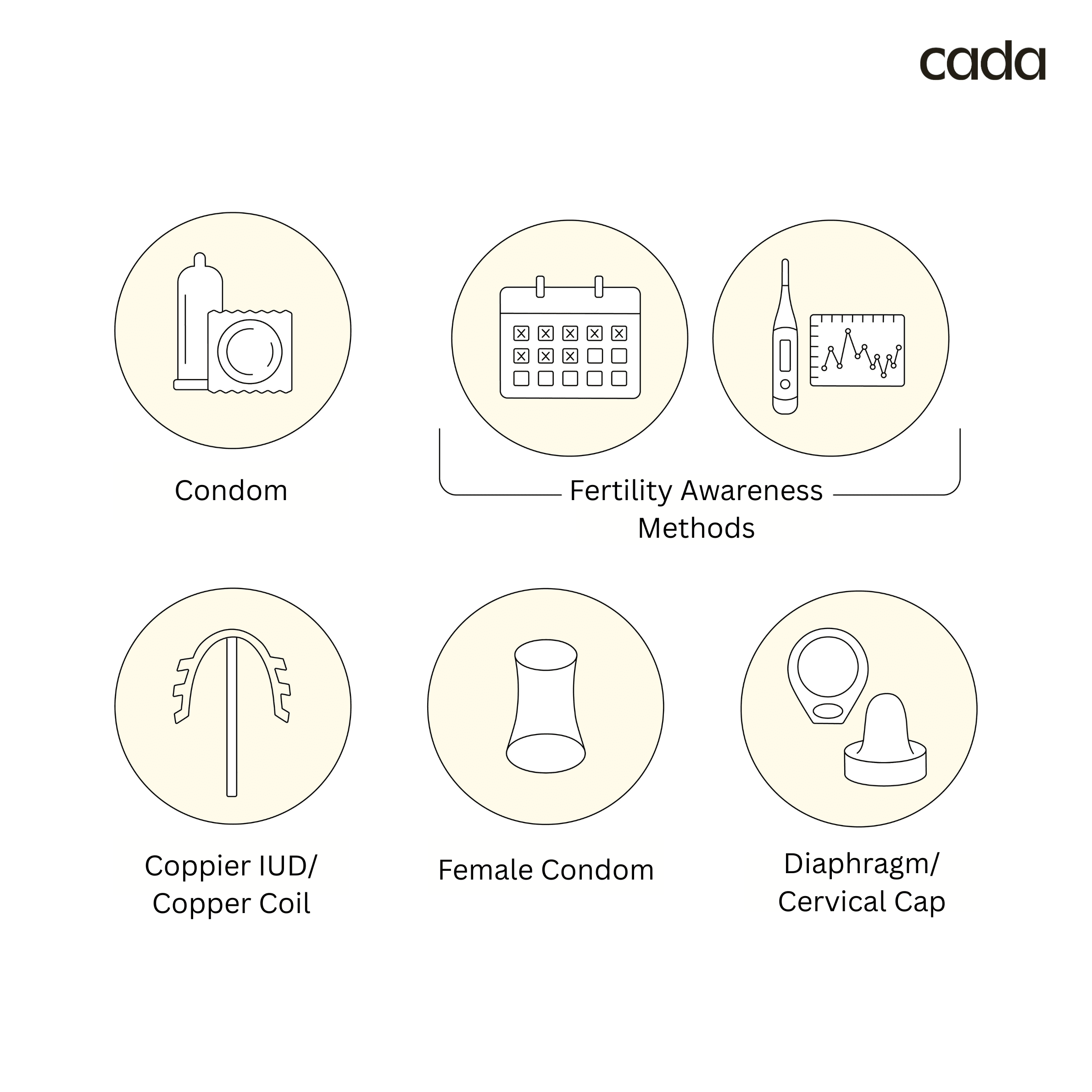
Choosing the right birth control option depends on your health history, lifestyle, and reproductive goals. Your healthcare provider can help determine which method suits you best.
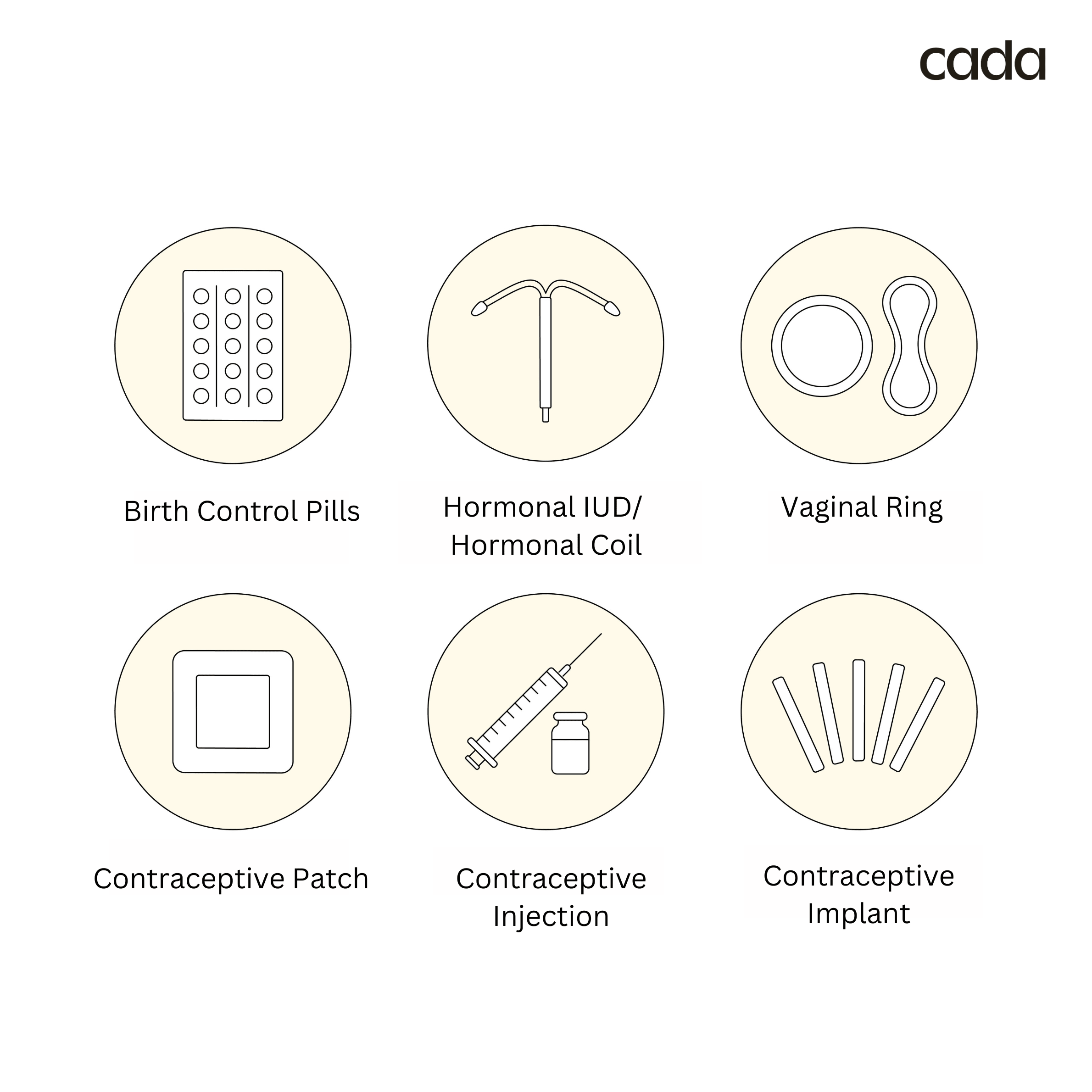
Hormonal Methods
Hormonal birth control methods work primarily by releasing synthetic versions of estrogen and progestin—hormones that regulate the menstrual cycle. These hormones prevent ovulation, thicken cervical mucus to block sperm, and thin the uterine lining to reduce the chances of a fertilized egg implanting.
The use of birth control pills and other hormonal methods gives your body the signal that it is in the post-ovulation phase, making further ovulation unnecessary. This mechanism is especially effective with consistent and correct use.
Some common types include:
- Combined contraceptive pills (contain both estrogen and progesterone)
- Progestin-only pills (also called the "mini pill")
- Hormonal coil (IUS): A T-shaped plastic device inserted into the womb, effective for several years.
- Contraceptive injections: Also known as the three-month injection.
- Vaginal rings: A soft ring placed inside the vagina for three weeks at a time.
- Hormonal patches: A skin patch worn for a week at a time (not applied to the breasts).
- Hormonal implants: A small rod placed under the skin, releasing progestogen for up to three years.
How Do These Methods Prevent Pregnancy?
Non-Hormonal Contraceptives
These methods work by physically preventing sperm from reaching and fertilising the egg, either by blocking entry to the cervix or altering the environment in the uterus or fallopian tubes.
Hormonal Contraceptives
Most hormonal methods prevent ovulation by releasing steady levels of progestogen. This tells the body it's already past ovulation, so no egg is released.
They also thicken the cervical mucus, making it harder for sperm to pass through the cervix – providing a double layer of protection and high effectiveness.
Note: Some hormonal methods, like the hormonal coil, primarily work by thickening cervical mucus and may not fully suppress ovulation. Effectiveness can also drop if methods are not used correctly – for example, forgetting to take the pill at the same time each day.
What Is the Pearl Index?
The Pearl Index indicates how many out of 100 women using a particular method for one year will become pregnant:
- Least effective: Withdrawal method (index 4–18)
- Most effective: Hormonal implant (index 0.1–0.9)
What Happens to Your Menstrual Cycle on Hormonal Birth Control?
Contraceptive use, especially with progestin-only or combined contraceptive pills, typically suppresses the natural cycle of the ovaries. This means no egg matures and ovulates, and the womb lining doesn’t thicken in preparation for pregnancy. As a result:
- You may not ovulate
- Your uterine lining remains thin
- Periods may become lighter, more regular, or stop entirely
Many contraceptive pills include a pill-free week, during which withdrawal bleeding occurs, but this is not the same as a natural period.
Common Side Effects of Hormonal Contraceptives
As with any medication, hormonal birth control can cause side effects. Every person reacts differently, but some commonly reported side effects include:
- Cramping
- Breast tenderness or enlargement
- Weight gain
- Nausea
- Acne
- Loss of libido
- Mood swings, including anxiety or depression
Coming Off Hormonal Birth Control: What to Expect
When you stop hormonal birth control, your cycle usually resumes within a few weeks.
In one study involving 187 women who stopped taking the contraceptive pill after continuous use (without withdrawal bleeding), 96.7% had their periods return spontaneously within 90 days, while a further 2% became pregnant during that time.
Another study found that 95% of women who had taken oral contraceptives for more than 40 cycles became pregnant within a year of stopping, compared to 90.5% of women who had used this form of birth control for just one to six cycles.
This suggests that long-term use of hormonal contraceptives is not associated with fertility problems.
A pregnancy test can help clarify if delayed menstruation after stopping birth control is due to early pregnancy.
Emergency Contraception and Fertility: Myths and Facts
Emergency contraception methods such as Plan B (a progestin-based morning-after pill) or an emergency copper IUD do not cause infertility. These are designed for short-term use after unprotected sex to prevent ovulation or fertilisation.
However, they are not recommended as a regular method of birth control due to reduced effectiveness with typical use and potential for side effects like nausea, cramping, or irregular bleeding.
How Quickly Does Fertility Return?
- Most women resume menstruation within a few weeks.
- A study found that 96.7% of women had a natural period within 90 days of stopping the pill.
- Another study showed that 95% of long-term pill users conceived within a year – slightly higher than those who had used it only briefly.
Not Ovulating After Birth Control? What You Can Do Next
Hormonal contraception is an effective method to prevent unintended pregnancy, mainly by stopping ovulation or thickening cervical mucus. If you're thinking about getting pregnant, rest assured that your fertility typically returns soon after stopping hormonal contraceptives, even after many years of use.
However, if your cycle remains irregular months after stopping, or you’re not ovulating, this could indicate an underlying issue worth discussing with your gynaecologist or a fertility specialist.
If you’ve been trying to conceive without success or are concerned about irregular ovulation, our compassionate fertility team at our fertility clinic in Zurich is here to help.
Book your personalized fertility consultation today to receive expert evaluation and guidance tailored to your unique situation.
FAQs on Hormonal Contraception and Fertility
Can Birth Control Cause Infertility or Birth Defects?
There is no scientific evidence that hormonal birth control causes infertility or bears an increased risk of birth defects. Most forms of hormonal contraception, including oral contraceptive, do not have long-term effects on fertility.
However, some conditions that were masked during contraceptive use—such as PCOS or endometriosis—may resurface after stopping, and these could impact fertility.
Can I use birth control while breastfeeding?
Yes, but some types are more suitable than others. Estrogen-containing contraceptives may reduce your milk supply. Progestin-only pills, hormonal IUDs, and contraceptive implants are generally considered safe during breastfeeding.
What should I know about wellness after stopping hormonal contraception?
Coming off hormonal birth control is a good opportunity to observe your natural cycle again. To support your wellness, focus on:
- Regular physical activity
- A balanced, nutrient-rich diet
- Managing stress levels
- Ongoing communication with your healthcare provider
Why is my period irregular after stopping the pill?
It's common for your cycle to be irregular after stopping contraceptive pills, especially if you had conditions like PCOS before. The pill may have masked these issues by creating regular bleeding patterns. Once you stop, your natural cycle—including any irregularities—can return.
When should I talk to a healthcare provider about my fertility?
If your period hasn’t returned or you haven’t become pregnant after:
- 12 months of trying (under age 35), or
- 6 months (age 35 and older),
you should consult a healthcare provider or a fertility specialist in gynecology.
What kind of tests might be recommended?
Your provider may:
- Check hormone levels
- Test for ovulation
- Rule out other causes like an ectopic pregnancy or ovulatory disorders







