Anti-Müllerian hormone (AMH) is a key indicator of your ovarian reserve and fertility. A blood test can easily determine your AMH levels.
Key Facts About AMH Levels
- Anti-Müllerian hormone levels correlate with your ovarian reserve.
- A high AMH levels indicate many eggs and may suggest polycystic ovary syndrome (PCOS).
- Lower levels suggest a reduced ovarian reserve or the onset of menopause.
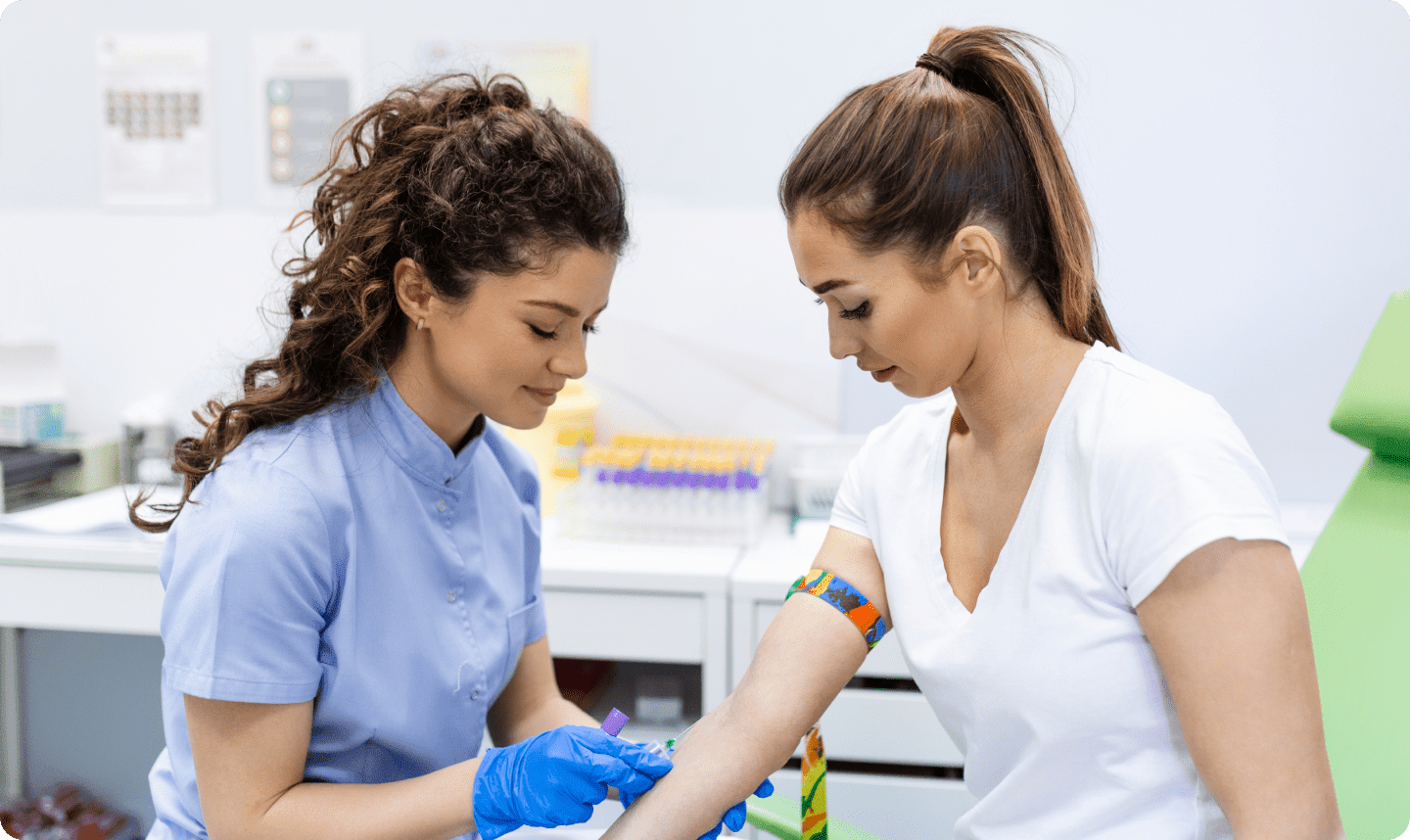
- The AMH level can be measured with a simple blood test.
- AMH plays a crucial role in sexual differentiation.
Important Indicator for Ovarian Reserve
The Anti-Mullerian hormone (AMH) is a glycoprotein that plays a crucial role in endocrinology and gynecology. It is a primary indicator of ovarian reserve, which refers to the number of eggs remaining in a woman's ovaries.
Ovarian reserve not only reflects the number of eggs but also their quality, which is influenced by the granulosa cells surrounding the developing follicles. These cells play a key role in supporting egg maturation and the overall health of the ovarian follicles.
If you want to know how many eggs remain in your ovaries, an AMH blood test may be helpful. Along with hormones like estrogen and progesterone, AMH is one of the key markers used to assess fertility and the chances of pregnancy.
In this article, you'll learn why AMH levels are tested, what they reveal about your fertility, and why they cannot be the sole reference for fertility evaluation.

Why AMH Levels Are Important
- Predicting Ovarian Reserve: The more ovarian follicles present, the higher the levels of AMH. A high AMH level indicates a greater number of remaining eggs, while a low level suggests a reduced egg count in the ovaries.
- Impact on Natural Conception: A reduced ovarian reserve can decrease the likelihood of natural conception due to fewer viable eggs being available.
- IVF Success Prediction: AMH levels provide insight into ovarian function and ovarian response during ovarian stimulation, such as in vitro fertilization (IVF). Poor response to hormonal stimulation often correlates with low AMH levels and fewer eggs.
- Timing Family Planning: AMH levels can help women decide when to start planning their family. A low AMH level may indicate that ovarian reserve is declining, making it more challenging to conceive naturally. Women who are not ready for pregnancy might consider options like egg freezing (fertility preservation).
- Sexual Differentiation: AMH is produced in Sertoli cells of the embryonic testes during fetal development in males. It causes the regression of the Müllerian ducts, which would otherwise develop into internal female reproductive organs. Without AMH, the Müllerian ducts persist, leading to the formation of female reproductive organs even in male fetuses (XY chromosomes).
What Does a High AMH Level Mean?
- High Ovarian Reserve: A high AMH level suggests that a woman has a large number of mature eggs in her ovaries. This is often seen as a positive sign for fertility since there are more potential eggs available for fertilization.
- Polycystic Ovary Syndrome (PCOS): In some cases, very high AMH levels may indicate PCOS, a hormonal disorder that can affect fertility. Hormonal treatment can help regulate the menstrual cycle and stimulate ovulation in women with PCOS.
What Does a Low AMH Level Mean?
- Low Ovarian Reserve: A low AMH level indicates that the egg supply in the ovaries is lower than expected, which may reduce the chances of natural conception and indicate a diminished ovarian reserve.
- Early Menopause: As women approach menopause, AMH levels naturally decrease due to the decline in ovarian reserve.
- Causes of Reduced Ovarian Reserve: In addition to age, other factors such as chemotherapy, radiation, ovarian surgery, or certain genetic disorders can lead to reduced ovarian reserve and lower AMH levels.
Learn more about the implications of low AMH levels in this podcast:
How is AMH Measured?
AMH is usually determined through a blood test taken from a vein in your arm. The blood sample is sent to a laboratory where the concentration of AMH in the blood serum is measured.
Anti-Mullerian hormone levels are relatively stable and can be measured at any time during the menstrual cycle. However, it is recommended to have the blood test during the first half of the cycle (follicular phase), as AMH levels are slightly higher at this time. After ovulation, AMH levels typically decrease.
If you're using hormonal contraception, your AMH test results may be about 30% lower. It's advisable to wait 2-3 menstrual cycles after stopping contraception before testing your AMH levels.
When Should AMH Be Measured?
AMH hormone levels are minimally higher at the beginning of the cycle and may show a slightly higher value compared to the second half, but this difference is not significant for determining the best time for AMH measurement. Several studies support this finding.
One study showed that AMH levels did not show consistent fluctuations during the cycle, unlike FSH, LH, and estradiol levels. The researchers concluded that AMH is a reliable, cycle-independent marker of ovarian reserve.
Another study from 2019 showed that AMH levels are higher in the follicular phase (the first half of the menstrual cycle) than in the luteal phase. However, these fluctuations were not significant enough to change the timing of AMH measurement during the cycle in clinical practice.
How Does AMH Impact My IVF Treatment?
A low AMH level may reduce the success rates of IVF because it indicates a lower ovarian reserve. However, it's important to note that AMH is just one factor in fertility evaluation. Other factors, such as egg quality, uterine lining, the woman's age, and additional fertility factors, also play a significant role. A higher AMH level often corresponds with a greater number of eggs retrieved and a higher chance of IVF success.
However, in some cases, high AMH levels may lead to a higher ovarian response during ovarian stimulation, which could increase the risk of Ovarian Hyperstimulation Syndrome (OHSS). This condition can occur when the ovaries respond too strongly to stimulation, leading to enlarged ovaries and fluid buildup. Women with higher AMH levels, often due to PCOS, may be at a higher risk of developing OHSS during an IVF cycle.
A study showed that AMH is not a decisive factor in IVF success for younger women (under 36). However, for women over 36, AMH can serve as a predictive factor.
Limitations of AMH Testing
While AMH levels are a helpful indicator of female fertility, there are key limitations:
- Not the Only Factor: Female fertility depends on many factors, not just ovarian reserve. Although AMH provides insights into the quantity of eggs, egg quality, the health of the uterus, and other health aspects are also important.
- Individual Differences: Every woman is unique, and interpreting AMH levels should always consider individual circumstances. A low AMH level does not necessarily mean infertility.
- Age-related Changes: AMH levels naturally decrease with age due to the diminishing number of follicles, which is completely normal.
Takeaway: AMH Levels Are Just One Part of the Picture
If you're wondering whether low or high AMH levels, such as in the case of polycystic ovarian syndrome (PCOS), are the reason for your infertility, or if you still have time to wait on your fertility goals, ovarian reserve testing measuring key hormones like estrogen, progesterone, AMH, FSH, and LH can provide valuable information.
AMH levels are an important indicator that can help assess female fertility. They provide insights into ovarian reserve and can assist in family planning decisions and fertility treatments.
However, it's important to remember that AMH is just one piece of the fertility puzzle. Factors like the patency of the fallopian tubes and sperm quality also play critical roles. Women with fertility concerns should always consult with a fertility specialist for a comprehensive evaluation.
At our fertility clinic in Zurich, we test your AMH levels and other hormones as part of our fertility test. Want to learn more? Book your appointment today.
Frequently Asked Questions About AMH Levels
How High Should My AMH Level Be to Get Pregnant?
A "normal" AMH level is approximately 0.7-8 nanograms per milliliter, with values between 1.0 and 3.0 ng/ml being ideal for natural conception. However, AMH levels can fluctuate with age and vary from woman to woman. The following table shows approximate normal AMH levels by age:
| Age | AMH Level |
|---|---|
| 25 Years | 3.0 ng/ml |
| 30 Years | 2.5 ng/ml |
| 35 Years | 1.5 ng/ml |
| 40 Years | 1.0 ng/ml |
| 45 Years | 0.5 ng/ml |
Which Other Blood Tests Should Be Done?
Along with AMH, tests for estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) should be conducted to provide a comprehensive fertility assessment. Additional tests, such as iron, vitamin D, or thyroid-stimulating hormone (TSH), may also be helpful.
Can I Improve My AMH Levels?
Unfortunately, there's no way to directly increase your AMH levels. Currently, no medications or treatments can restore ovarian reserve or increase the number of eggs.
What is the AMH Level in Menopause?
AMH levels lower than 0.1 ng/ml typically indicate menopause.







